Your cart is currently empty!
Blood Clot Warning Signs Doctors Say You Should Never Dismiss
Something shifts inside your body without warning. A dull ache starts in your calf. Swelling appears in one leg but not the other. Your skin takes on an unusual reddish tint. Most people dismiss these signs as minor inconveniences, attributing them to a pulled muscle or sleeping in an awkward position.
Sometimes these symptoms mean exactly that. Other times, they signal something far more serious.
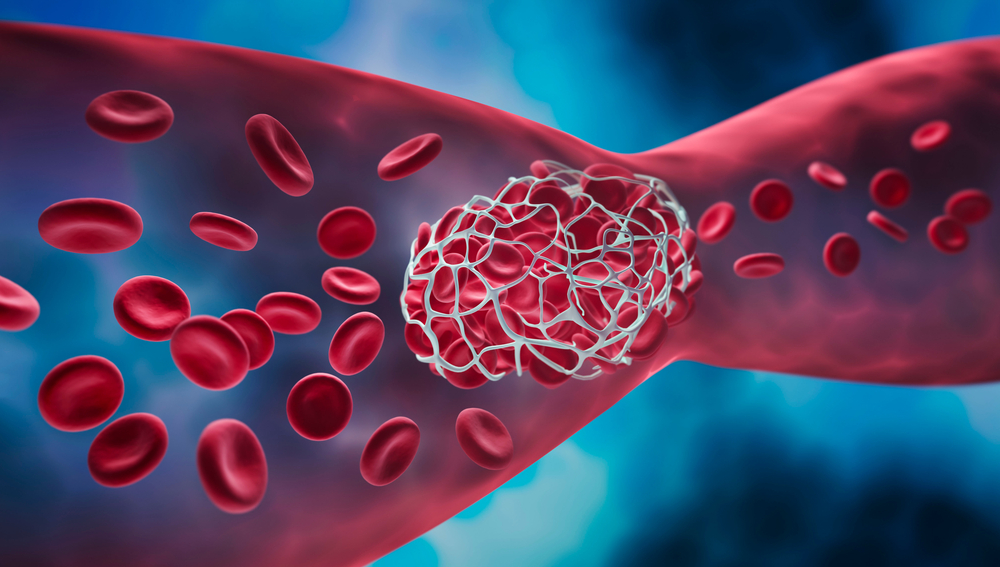
Blood clots form when platelets, proteins, and blood cells stick together into a gel-like mass. Your body creates these masses as part of its natural healing process when blood vessels get damaged. But clots don’t always form where they should, and they don’t always dissolve when their job is done.
How Blood Turns Solid
Blood clotting represents one of your body’s most elegant defense mechanisms. When a vessel sustains damage, platelets rush to the scene. Clotting factors join them, working together to create a fibrin clot that seals the injury and allows healing to begin.
“Your body has two blood vessel systems: arteries and veins,” Dr. Johnston explains. “They form clots for different reasons.” Arterial clots typically develop where vessel walls have been damaged by conditions like atherosclerosis. Venous clots often form when blood flow slows or stops, allowing platelets and clotting factors to accumulate.
Understanding how your body creates these masses helps explain why certain conditions put you at higher risk.
Who Faces Higher Risk

Genetic conditions and family history play major roles in blood clot formation. If your parents or siblings developed clots, your chances increase. Certain inherited disorders affect how your blood clots, making you more susceptible to developing dangerous masses.
Immobility ranks among the most common risk factors. Long flights, extended bed rest after surgery, or sitting at a desk for hours without moving allow blood to pool in your legs. Cancer and its treatments can alter your blood chemistry, increasing clot formation. Recent surgeries, particularly orthopedic procedures, create conditions where clots form more easily.
Pregnancy changes how blood clots as your body prepares for childbirth. Obesity affects blood flow patterns. Hormonal contraceptives can alter clotting factors in some women. Age matters too, with risk climbing after 40.
Silent Threats That Turn Deadly
Clots that go undetected pose severe dangers. A clot forming in a deep leg vein might seem like a localized problem, but these masses don’t always stay put.
“A clot in a deep leg vein can break off and travel to your lungs, causing a potentially fatal pulmonary embolism,” Dr. Johnston warns. When a clot reaches your lungs, it blocks blood flow and prevents oxygen from reaching vital organs. Large pulmonary embolisms can kill within minutes.
Clots that travel to the brain cause strokes. Blood flow stops to the brain tissue, and cells begin dying. Without rapid treatment, strokes lead to permanent disability or death. Post-thrombotic syndrome develops in some people after deep vein thrombosis, causing chronic pain, swelling, and skin discoloration that lasts for years.
Early detection changes outcomes dramatically. Recognizing symptoms and seeking immediate medical attention can prevent these complications.
1. Pain That Refuses to Quit

One of the first warning signs appears as unexplained pain in a specific area. Blood clot pain differs from typical muscle soreness in distinct ways.
“Trapped blood puts pressure on tissue and nerves, causing a deep ache or cramp that doesn’t go away,” Dr. Johnston explains. Unlike a pulled muscle that improves with rest and over-the-counter pain relievers, clot pain persists. It might feel like a severe charley horse that never releases, or a dull throbbing sensation that intensifies when you stand or walk.
Muscle strains respond to ice, elevation, and basic pain medication. Blood clot pain resists these treatments. If pain in your leg, arm, or hip continues for days without improvement, medical evaluation becomes necessary.
2. One Leg Swells While the Other Stays Normal
Swelling that affects just one limb raises immediate red flags. When a clot forms in a vein, it acts like a dam. Blood can’t drain properly from the limb, and fluid leaks into the surrounding tissue.
“A clot in a vein stops blood from draining,” Dr. Johnston says. “That causes fluid to leak into the tissue.” Measuring your limb helps track changes. Wrap a tape measure around the thickest part of your calf or thigh, then compare it to the same spot on your other leg. A difference of more than two centimeters suggests something serious.
Record measurements daily at the same time. If swelling increases or persists beyond a few days, call your doctor.
3. Skin Tells Its Own Story

Skin changes accompany many blood clots. Affected areas might turn red, purple, or take on a bluish tint. Blocked blood flow prevents normal circulation, causing these color changes.
Warmth often appears alongside discoloration. Touch the affected area and compare it to the surrounding skin or the same spot on your other limb. Your body sends inflammatory signals to the area, causing localized warmth and skin discoloration.
Inflammation represents your immune system’s attempt to address the problem. While inflammation helps fight infections, it also serves as a warning signal that something has gone wrong inside your blood vessels.
4. Veins That Look Different
Veins that suddenly appear larger or more prominent can indicate clotting. “Enlarged and puffy veins in the leg can be early signs of DVT,” Dr. Johnston says. Deep vein thrombosis gets its name from clots forming in veins deep beneath the skin’s surface.
When a clot blocks blood flow, the vein swells. You might see what looks like a thick cord running under your skin. These veins feel tender when touched and appear harder than normal veins. Surrounding skin might feel warm or look red.
Some people notice their veins look more visible than usual, with a rope-like quality that wasn’t there before. Any sudden change in how your veins look or feel warrants a doctor’s visit.
5. When Breathing Becomes a Struggle

Respiratory symptoms signal that a clot has traveled to your lungs. Pulmonary embolism causes sudden shortness of breath that seems to come from nowhere. One moment you’re breathing normally, the next you can’t catch your breath.
Chest pain accompanies the breathing difficulty. Sharp, stabbing sensations worsen when you take deep breaths. Your heart races as it tries to compensate for blocked blood vessels. Some people cough up blood.
That could mean a clot has traveled to your lungs, a pulmonary embolism. Pulmonary embolism demands immediate emergency care. Call 911 or have someone drive you to the nearest emergency room. Minutes matter with this condition.
6. Stroke Symptoms Demand Fast Action
Blood clots in the brain cause strokes. Symptoms appear suddenly and require immediate recognition. Weakness or numbness affects one side of your face, arm, or leg. Speech becomes slurred or difficult. Vision problems develop. Severe headaches strike without warning.
Remember FAST when evaluating potential stroke symptoms. Face drooping on one side, arm weakness when trying to raise both arms, speech difficulties, and the need to call emergency services immediately.
Quick treatment can make a huge difference. Doctors have a narrow window to administer clot-dissolving medications. Treatment within 4.5 hours offers the best chance for good outcomes with minimal disability. Beyond that window, options become limited and results less favorable.
7. Coughs and Fevers as Hidden Clues

Less obvious symptoms sometimes appear with lung clots. A persistent cough that won’t respond to usual treatments might indicate blocked blood flow to part of your lung.
If a lung section can’t get blood because of a clot, it can irritate, coughing, or bleeding in the airways. Fever sometimes develops as your body responds to the clot with inflammation.
Pay attention when these symptoms occur alongside others. A cough combined with leg swelling or arm pain creates a more complete picture. Individual symptoms might have innocent explanations, but combinations suggest something more serious.
Getting the Right Diagnosis

Medical evaluation starts with a physical examination and medical history. Your doctor asks about symptoms, when they started, and whether you have risk factors for clotting.
If you think you might have DVT in your leg, see your doctor fast. Dr. Johnston advises. Several tests help confirm or rule out blood clots. Ultrasound uses sound waves to visualize blood vessels without surgery. D-dimer blood tests measure substances released when clots break down. Venography involves injecting contrast dye that shows up on X-rays, allowing doctors to see exactly where clots form.
CT scans and MRIs provide detailed images of different body areas. Your doctor chooses tests based on where they suspect a clot might be hiding.
Lowering Your Risk Starts Now
Prevention beats treatment. Move around as soon as possible after surgery or an illness that requires bed rest. During long flights or car trips, stand and walk every few hours. Flex your ankles and knees while seated to keep blood flowing.
Compression stockings help prevent pooling in leg veins during long flights or after surgery. Regular physical activity keeps blood moving through your vessels. Maintaining a healthy weight reduces strain on your circulatory system. Quit smoking, which damages blood vessels and increases clot risk.
Lowering your risk starts with awareness. People at high risk might need blood thinners as preventive medication. Discuss your individual risk factors with your doctor.
Taking Symptoms Seriously
Blood clots can form without obvious warning signs. Recognizing the seven key symptoms gives you the knowledge to seek help when it matters most. Pain that won’t quit, swelling in one limb, skin changes, visible vein differences, breathing difficulties, neurological symptoms, and persistent coughs all deserve medical attention.
Fast action saves lives. If you notice these warning signs, contact your doctor immediately or seek emergency care. Early treatment prevents complications and improves outcomes dramatically. Your awareness and willingness to act quickly can make all the difference.
