Your cart is currently empty!
Baby girl grows ‘micropenis’ after absorbing testosterone from laying on her father’s chest
In an age where modern medicine has made it easier than ever to manage hormonal imbalances, a growing number of men and women are turning to hormone replacement therapies for support with aging, fatigue, and sexual health. But a recent case out of Sweden serves as a sobering reminder that even routine treatments can carry unintended consequences — especially when children are involved.
When a baby girl began showing signs of masculinized genitalia after frequent skin-to-skin contact with her father, doctors uncovered an unexpected culprit: residual testosterone gel from his prescribed therapy. The case, documented by Swedish pediatric endocrinologists, is not the first of its kind — and it points to a larger, underrecognized risk in homes where hormone therapies are in use.

When Hormone Therapy Poses an Unseen Risk: The Medical Case
Skin-to-skin contact between parents and newborns is widely recommended for its psychological and physiological benefits, including bonding and temperature regulation. However, in a rare and concerning case reported by Swedish doctors, this otherwise nurturing practice had unexpected consequences when a 10-month-old baby girl developed virilized genitalia after regular contact with her father’s bare chest. The father, as it turned out, was using a prescription testosterone gel — a topical medication intended to treat symptoms of low testosterone in men.
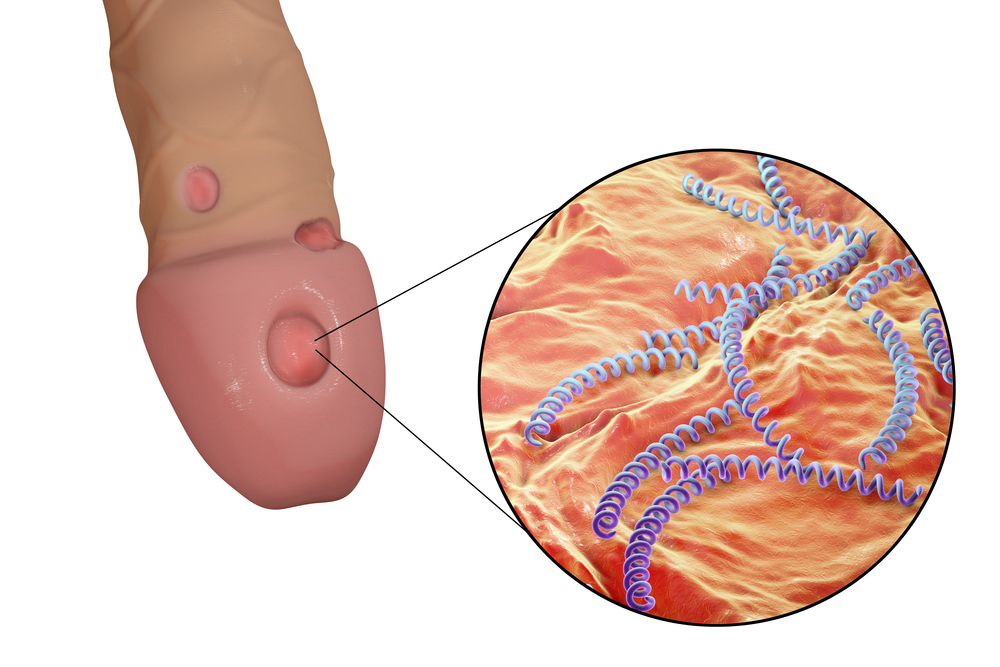
According to Professor Jovanna Dahlgren, a pediatric endocrinologist at Sahlgrenska University Hospital in Gothenburg, the girl’s exposure to residual testosterone transferred from her father’s skin led to a measurable hormonal imbalance. Clinically, the child exhibited signs of virilization — a condition where females develop male secondary sexual characteristics. Her clitoris enlarged significantly, resembling a small penis, and the labia partially fused, mimicking the appearance of a scrotum.
Though media outlets described the resulting appearance as a “micropenis,” this is a misnomer. A true micropenis is a medical diagnosis reserved for males with unusually small penile development due to hormonal deficiencies during fetal growth. In this case, the more accurate term is clitoral hypertrophy induced by exogenous androgen exposure.
Blood tests confirmed elevated testosterone levels in the infant, and the symptoms began to regress once the father’s use of the gel — and unintentional contact with his daughter — ceased. This case adds to a small but growing body of similar incidents that raise urgent questions about how potent and transferable hormone treatments can be, especially through skin contact.
Professor Dahlgren noted that she has tracked at least half a dozen such cases over recent years. In another instance, a 10-year-old boy reportedly developed breast tissue after prolonged exposure to estrogen cream his mother was using. “I don’t think people always understand how potent these treatments are,” she told Göteborgs-Posten. “The parents become completely desperate when they understand what has happened.”

A Growing Trend, A Growing Risk: Hormone Therapies in Everyday Homes
The incident in Sweden is not an isolated anomaly. As hormone replacement therapies become increasingly common — particularly testosterone replacement therapy (TRT) for men — the potential for accidental secondary exposure is rising in tandem. Originally developed to treat clinically low testosterone levels or hypogonadism, TRT is now being marketed more aggressively to men experiencing general symptoms such as fatigue, low libido, or muscle loss. Some clinics promote it to men as young as 30, positioning the treatment as a way to stave off the so-called “manopause.”
In the UK alone, the National Health Service (NHS) reportedly prescribes testosterone therapy to over 80,000 men, and that figure doesn’t account for the growing number of men receiving private prescriptions through telehealth services and wellness clinics. With such widespread use, the domestic sphere has become a site of inadvertent risk — especially for infants and children.
These risks are not merely theoretical. In 2023, the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) received reports of a child experiencing “increased growth and genital enlargement” after being exposed to a parent’s testosterone gel. The case prompted regulators to require manufacturers to include explicit warnings about the potential for secondary exposure. Instructions now emphasize the need for users to wash their hands thoroughly after application and avoid skin-to-skin contact with children — especially within a few hours of applying the gel.
Similar cautionary guidelines apply to hormone therapies used by women, such as estrogen creams and gels prescribed for menopausal symptoms. These too carry the risk of transferring potent hormones to others through casual physical contact.
Despite regulatory efforts, awareness of these precautions remains low. As Professor Dahlgren emphasized, many parents simply don’t realize how easily hormone products can be absorbed through the skin or transferred via residue on bedding, clothing, or even unwashed hands. This knowledge gap underscores the need for clearer public messaging and stronger safeguards in prescribing practices — particularly when young children are present in the home.

The Powerful Role of Hormones in Early Development
Hormones, especially sex hormones like testosterone and estrogen, play a tightly regulated role in human development — even from before birth. In typical development, testosterone contributes to male sexual differentiation in utero, guiding the formation of male genitalia and other secondary sex characteristics. For females, whose bodies produce far lower levels of testosterone, the presence of elevated androgens — particularly during sensitive developmental windows — can disrupt this natural trajectory.
Children, and especially infants, are uniquely vulnerable to hormonal imbalances because their endocrine systems are still developing. Unlike adults, their bodies have not yet built the regulatory mechanisms needed to buffer external hormonal influences. When a child is exposed to an exogenous hormone like testosterone — even through skin contact — it can override the body’s own signals and trigger inappropriate physiological responses.
In the Swedish case, the baby girl’s exposure led to virilization: the abnormal development of male physical traits in a female child. While the physical changes in her genitalia were the most visible signs, excessive testosterone in children can also affect brain development, bone growth, and potentially long-term reproductive health if the exposure is sustained.
According to the Endocrine Society, exposure to endocrine-disrupting chemicals or medications during critical periods of growth — such as infancy or early childhood — may have permanent effects on sexual development, metabolic function, and even behavior. Though short-term exposures like in this case may resolve once the source is removed, prolonged or repeated contact could carry longer-term consequences that are not yet fully understood.
Gaps in Awareness: What Regulation Alone Can’t Fix
While medical regulators have begun to take action in response to cases like the Swedish incident, the reality is that guidelines often lag behind growing consumer trends — and enforcement depends heavily on public awareness and individual responsibility. In the UK, following reports of testosterone-related side effects in children, the Medicines and Healthcare products Regulatory Agency (MHRA) issued new labeling requirements mandating that testosterone gels include clear warnings about avoiding skin-to-skin contact with children. But these measures, though important, are only as effective as their communication and comprehension.
In clinical settings, patients prescribed hormone replacement therapy — whether for menopause, hypogonadism, or age-related decline — should be counseled thoroughly on how to use the medications safely. This includes not only applying the medication to covered areas but also washing hands immediately afterward, allowing the gel to dry before dressing, and ensuring treated areas do not come into contact with others, especially young children. Unfortunately, anecdotal evidence and recurring case reports suggest that many patients do not fully understand these precautions or may become complacent over time.
Moreover, as hormone therapy becomes increasingly available through private providers and online platforms, some patients may receive prescriptions without the same level of face-to-face consultation or ongoing monitoring typical of NHS treatment. This convenience can come at the cost of oversight. While online services may offer accessibility, they sometimes lack the robust patient education that accompanies traditional medical care.
Professor Jovanna Dahlgren emphasized that parents in these cases are often shocked and distressed, not because they ignored warnings — but because they never knew the risk existed. “The parents become completely desperate when they understand what has happened,” she told Göteborgs-Posten. This statement speaks not only to the emotional toll but to a broader systemic issue: the failure to effectively translate regulatory policies into practical, accessible information for families navigating complex medical therapies at home.
Education campaigns targeting both healthcare professionals and the general public — especially parents — are vital. It’s not enough to rely on fine print or package inserts. Hormone treatments are potent medical interventions, and as their use becomes more widespread, the safeguards must extend beyond the clinic and into the home.
A Teachable Moment: Protecting Children in a Medicated World
The case of a baby girl developing virilized genitalia from unintentional testosterone exposure is more than a medical anomaly — it’s a teachable moment that highlights the often-overlooked risks of modern pharmaceutical use in family environments. As hormone replacement therapies become increasingly accessible and normalized, especially through direct-to-consumer marketing, it’s crucial to reframe how we think about medication safety — not just for the user, but for everyone in their immediate surroundings.
Parents, caregivers, and anyone undergoing hormone therapy must understand that these medications do not exist in isolation. Transdermal products, by design, remain active on the skin for a period of time after application, making inadvertent exposure a real and preventable danger — particularly for infants and children whose bodies are still forming the blueprints for lifelong development.
This is not a call to shame or vilify those who use hormone treatments. When prescribed and monitored responsibly, these therapies can offer real improvements in quality of life. But they must be handled with the same vigilance one would apply to any potentially hazardous substance in the home — a locked medicine cabinet, proper hand hygiene, covered application areas, and proactive conversations with healthcare providers about safety protocols.
