Your cart is currently empty!
Scientists Just Won a Nobel Prize for Discovering How to Stop Your Immune System from Attacking You

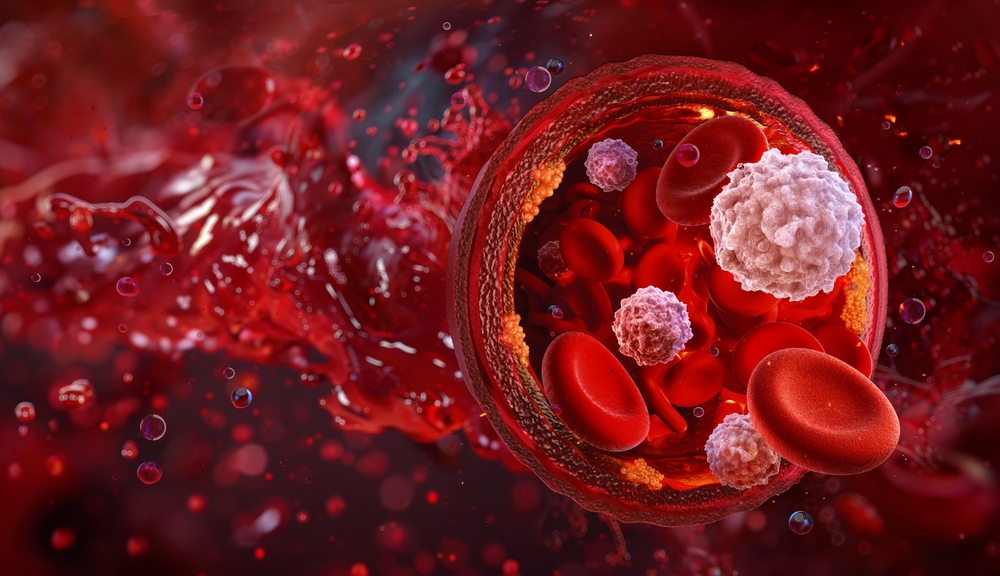
Every moment of every day, your body wages microscopic warfare. Thousands of viruses, bacteria, and microbes attempt to invade. Your immune system fights them off with precision. But here’s the catch: some of those protective soldiers can turn their weapons on you. For decades, scientists couldn’t explain why most people escape this friendly fire. Now three researchers have won the 2025 Nobel Prize in Physiology or Medicine for solving that puzzle.
Mary Brunkow, Fred Ramsdell, and Shimon Sakaguchi will share $1.1 million for discovering the immune system’s security guards. Regulatory T cells, as these guards are now called, prevent your body from attacking itself. Without them, autoimmune diseases would run rampant.
When Protection Becomes Destruction
Your immune system faces an impossible task. It must distinguish friend from foe among billions of cells. Many invaders have evolved to look like human cells, wearing molecular camouflage. One wrong move and your immune system could destroy healthy organs.
Scientists once believed they understood how this worked. During development, immune cells mature in an organ called the thymus. Cells that recognize the body’s own tissues get eliminated there. Researchers called this central tolerance and assumed it was enough.
A Japanese Researcher Takes a Risk

Shimon Sakaguchi made a career-defining choice in the 1990s. While most scientists had abandoned the idea of specialized immune suppressors, he pursued it. His colleagues at Aichi Cancer Center Research Institute in Japan had performed a strange experiment years earlier. When they removed the thymus from newborn mice, the immune system went haywire. Instead of becoming weaker, it attacked the mice’s own organs.
Sakaguchi saw something others missed. He isolated T cells from healthy mice and injected them into mice without a thymus. Results surprised him. Some T cells could protect against autoimmune disease. But helper T cells normally activate the immune system, not calm it down.
He spent over a decade searching for a way to identify these protective cells. In 1995, he published his findings in The Journal of Immunology. A specific class of T cells carrying both CD4 and CD25 proteins on their surface could suppress immune attacks. He had discovered regulatory T cells.
Most scientists remained skeptical. Proof would come from an unexpected source: sickly mice born during the Manhattan Project.
A Wartime Mystery

In the 1940s, researchers at Oak Ridge, Tennessee, studied radiation effects as part of atomic bomb development. Some male mice were born with scaly, flaky skin. Their spleens and lymph glands swelled to extreme sizes. They lived for only a few weeks.
Scientists named this strain “scurfy” and kept breeding it. Females could carry the mutation without getting sick because they had two X chromosomes. Males, with only one X chromosome, developed the full disease. Decades later, molecular biologists discovered that T cells were destroying these mice’s organs from within.
Mary Brunkow and Fred Ramsdell saw an opportunity. In the 1990s, they worked at Celltech Chiroscience, a biotech company developing treatments for autoimmune diseases. If they could find the genetic mutation causing the scurfy condition, they might unlock secrets about human autoimmune disorders.
They faced a daunting challenge. Mouse X chromosomes contain roughly 170 million DNA base pairs. Finding one mutation meant searching through a molecular haystack.
Six Years in the Desert
Brunkow and Ramsdell began their hunt. They narrowed the search area to 500,000 nucleotides. Then came the painstaking work of mapping that region in detail and comparing healthy mice to scurfy mice.
Gene by gene, they searched. Nineteen genes showed no differences. Only the twentieth and final candidate revealed the answer. Years of work paid off when they identified the mutation in a previously unknown gene. They named it Foxp3, after its similarity to a family of genes that regulate other genes.
Brunkow later described the ordeal plainly: “It was really a molecular slog, to get to that exact mutation. It was just a very small genetic alteration that results in quite a profound change in the immune system.”
Their 2001 paper in Nature Genetics revealed something else. A rare human disease called IPEX, which causes severe autoimmune symptoms in boys, stems from mutations in the human version of FOXP3. Boys with IPEX develop skin rashes, enlarged spleens and lymph nodes, and life-threatening complications. Brunkow and Ramsdell had connected mouse genetics to human disease.
Two Discoveries Become One
Labs around the world began connecting dots. In 2003, Sakaguchi proved that the FOXP3 gene controls regulatory T cell development. Other researchers confirmed it. Scientists could even transform regular T cells into regulatory T cells by switching on FOXP3 expression.
Markus Feuerer, an immunologist at the Leibniz Institute for Immunotherapy, put it simply: “Anyone who does not have an autoimmune disease, that’s because of these regulatory T cells.”
Peripheral immune tolerance, as this process is known, keeps your immune system from running wild after it eliminates threats. Regulatory T cells monitor other immune cells and tell them when to stand down. Without these guards, your body would tear itself apart.
An Off-Grid Winner
On October 6, 2025, the Nobel Committee tried to reach Fred Ramsdell. He was backpacking in Idaho’s wilderness, completely unreachable. Colleagues at Sonoma Biotherapeutics, where Ramsdell now serves as scientific adviser, couldn’t contact him all day. He learned of his Nobel Prize on Monday evening after hiking back to civilization.
Mary Brunkow, now at the Institute for Systems Biology in Seattle, got the call around 4 a.m. Cameras captured her emotional reaction to the news.
Sakaguchi, speaking at an Osaka University press conference, called the award “a happy surprise.” He thanked students and collaborators who made the research possible. “I was never working alone—there were people all over the world who shared similar ideas,” he said. “I see this award as one that represents all of those people who have contributed to this research alongside me.”
Nobel Committee Chair Olle Kämpe explained the significance: “Their discoveries have been decisive for our understanding of how the immune system functions and why we do not all develop serious autoimmune diseases.”
Medicine Gets New Tools
Cancer researchers have found that tumors recruit regulatory T cells as shields. These cells suppress immune attacks, letting cancer grow unchecked. Scientists are now developing ways to reduce or redirect regulatory T cell activity around tumors. If they can dismantle those shields, the immune system might access and destroy cancer cells.
Sakaguchi continues exploring how to fine-tune immune responses for cancer treatment. His work might help the body fight malignancies more effectively. Autoimmune disease treatment takes the opposite approach. Researchers want to boost regulatory T cell numbers. Clinical trials are testing interleukin-2, a substance that helps regulatory T cells thrive. Early studies suggest it might calm overactive immune systems in patients with autoimmune conditions.
Organ transplant patients face a different challenge. Their immune systems try to reject foreign organs. Interleukin-2 might help prevent rejection by strengthening the regulatory T cell population.
Engineered Solutions
Some researchers are taking a more direct approach. They isolate regulatory T cells from patients, multiply them in laboratories, and return them to the body. More security guards mean better immune control.
Cutting-edge techniques add another layer. Scientists can modify regulatory T cells with antibodies that act like address labels. These engineered cells travel to specific organs, such as transplanted kidneys or livers, and protect them from immune attack.
Jeff Bluestone, CEO of Sonoma Biotherapeutics, described the potential: “The ability to manipulate these cells so that they can become powerful, specific therapeutics is really the promise of the field.”
More than 200 clinical trials involving regulatory T cells are now registered worldwide. Companies like Sonoma, which Ramsdell co-founded, are developing engineered regulatory T cell therapies to dampen harmful inflammation.
Long-Awaited Recognition

Immunologists applauded the Nobel Committee’s decision. Carola Vinuesa, who studies autoimmunity at the Francis Crick Institute, called the laureates’ work “one of the immune system’s most critical regulatory mechanisms.”
Thomas Boehm of the Max Planck Institute of Biology expressed particular satisfaction that Mary Brunkow received recognition. “She has not always received the credit she deserves for her work,” he noted.
Adrian Liston of the University of Cambridge said he had been waiting years for this kind of recognition. “If you control the brakes to the immune system, it gives you the ability to turn the immune response up or to tone it down,” he explained.
Colleagues stressed the importance of curiosity-driven research. Basic science discoveries often take decades to reach clinical applications. Sakaguchi’s initial findings came in 1995. Brunkow and Ramsdell published in 2001. Only now are treatments reaching patient trials.
From Lab Bench to Patient Bedside

Regulatory T cell research has opened entire fields of medicine. Treatments for autoimmune diseases, cancer, and transplant complications all stem from these discoveries. Some therapies are already in late-stage clinical trials.
Patients with conditions from rheumatoid arthritis to inflammatory bowel disease might benefit. Cancer patients could see improved outcomes if researchers successfully target regulatory T cells around tumors. Transplant recipients might avoid rejection without harsh immunosuppressive drugs.
Decades of work by three scientists swimming against conventional wisdom have given medicine new weapons. Your body’s security guards, once unknown, now offer hope for millions facing immune-related diseases. And it all started with skeptical scientists, sick mice, and a refusal to accept that the immune system’s story was already complete.
