Your cart is currently empty!
Study Shows Women’s Brains Work Harder, Requiring More Sleep

For many, the feeling of exhaustion upon waking is a familiar struggle, yet research suggests that the weight of a busy day may leave a deeper mark on some than others. While a standard night of rest is often recommended as a universal health requirement, the complexity of modern cognitive demands points toward a biological disparity in how people recover. Recent scientific insights into brain activity and physiological resilience are shifting the conversation around rest, revealing why the simple act of closing one’s eyes for the night is a uniquely vital process for women.
The Science of Sleep and the Demands of Multitasking
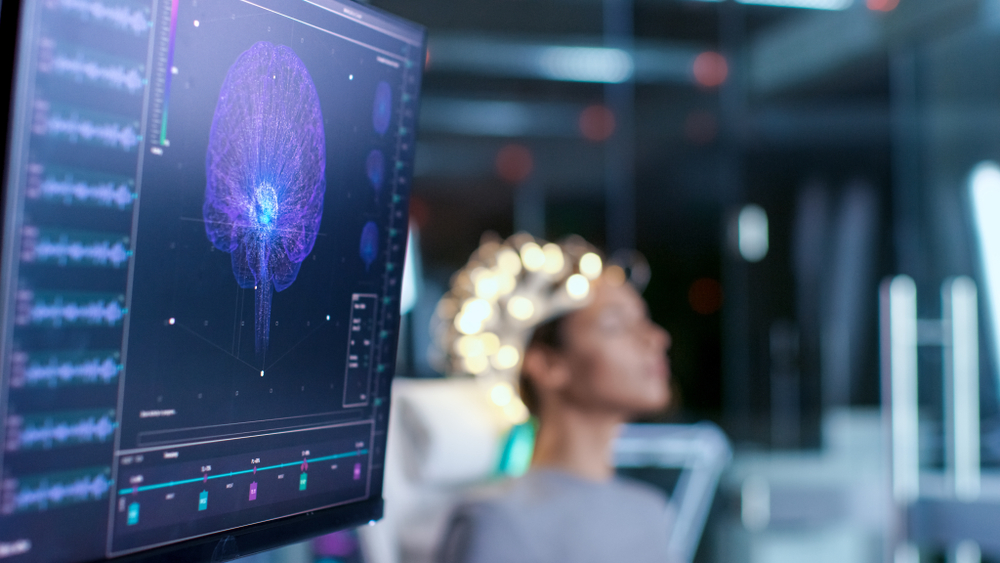
The daily mental load often feels heavy, but science suggests that for many women, the brain is working harder to manage concurrent responsibilities. Research from the Sleep Research Center at Loughborough University reveals that women generally require more sleep than men, driven by the specific ways they process information throughout the day. Professor Jim Horne, a leading sleep expert and former director of the center, points out that because women frequently multitask and remain flexible, they engage a larger portion of their actual brain during waking hours.
This high level of cognitive activity creates a greater physical demand for downtime. One of the primary functions of sleep is to allow the neural pathways to recover and repair themselves after exertion.

Professor Horne explains that the more a brain is used during the day, the more of it needs to rest to fully regenerate. His research, which monitored over 200 individuals, indicates that women need an average of 20 additional minutes of rest per night. This is not a matter of preference but a biological requirement for maintaining cognitive health.
When a brain is constantly shifting between different tasks and emotional demands, those extra minutes of sleep serve as a vital window for the recovery needed to handle the challenges of the following day.
Why Sleep Debt Costs Women More

While insufficient rest affects everyone, the physiological consequences of sleep deprivation appear to be more severe for women. Dr. Edward Suarez, an associate professor at Duke University School of Medicine, found that poor sleep quality is specifically linked to a higher risk of coronary heart disease, Type 2 diabetes, and hypertension in women. These findings suggest that a woman’s body reacts more intensely to the stress of exhaustion than a man’s does under similar conditions. Researchers identified elevated levels of fibrinogen and inflammatory biomarkers in sleep-deprived women, which act as internal signals of systemic stress.
Beyond the cardiovascular risks, the study noted that sleep-deprived women often experience higher fasting insulin levels, a factor that can complicate metabolic health and increase long-term disease risk. These physical markers are frequently accompanied by significant psychological distress. Professor Horne’s research supports this, noting that for women, inadequate rest is strongly associated with increased feelings of hostility, depression, and anger. This “short fuse” phenomenon is a documented reaction to neural fatigue, yet interestingly, these same emotional responses were not observed to the same degree in men who experienced similar sleep disruptions. This disparity highlights that for women, meeting the body’s demand for sleep is not a luxury, but a critical pillar of both physical health and emotional stability.
Barriers to Quality Rest

Despite the biological need for more rest, women often face unique hurdles that disrupt their sleep cycles. Research indicates that women frequently have a harder time falling back to sleep after being woken up, a struggle often attributed to a tendency to think and worry while lying in bed. This cognitive alertness, where the brain remains engaged in problem-solving or planning even during rest hours, creates a cycle of wakefulness that is difficult to break. Unlike the immediate “shut off” many men experience, a woman’s brain may continue to process the day’s events, making the transition to deep sleep much slower.
External factors and life stages further complicate this issue. Mothers, in particular, face significant sleep stumbling blocks, ranging from the physical discomforts and hormonal shifts of pregnancy to the ongoing care of young children. These interruptions are more than just a temporary nuisance; they fragment sleep and prevent the brain from reaching the deep, restorative stages required for full neural repair.
Furthermore, the modern environment, which is often filled with digital distractions and work-from-home demands, keeps the mind active late into the night. For many women, the challenge isn’t just finding the time to sleep, but overcoming the physiological and environmental barriers that keep a busy mind from truly switching off. These compounding factors mean that even when a woman is in bed for eight hours, the actual quality of that rest may be significantly diminished.
The Neurochemical Foundation of Sleep

Beyond external stressors, the quality of our rest is governed by a delicate balance of three primary neurochemicals: serotonin, melatonin, and acetylcholine. These components act as the biological clockwork that signals the body when to wind down and when to remain in restorative deep sleep. Serotonin is essential for regulating mood and serves as a vital precursor to melatonin, the hormone responsible for maintaining the circadian rhythm and signaling the body that it is time for rest. Without sufficient serotonin, the production of melatonin is hampered, leading to difficulties in falling asleep.
Meanwhile, acetylcholine plays a vital role in managing the transitions between different sleep stages, particularly during the dreaming phase of REM sleep. This chemical helps the brain navigate the complex architecture of rest, ensuring that transitions between light and deep sleep occur smoothly. When these chemical levels are disrupted by lifestyle factors, chronic stress, or diet, the ability to fall and stay asleep is compromised.
For many women, maintaining this chemical equilibrium is more difficult because of the high cognitive and physical demands previously discussed. A deficiency in these areas can lead to a persistent state of alertness that defies even the most disciplined bedtime schedule.
Recognizing that sleep is a chemical process as much as a behavioral one allows for a more comprehensive approach to rest. Addressing these internal imbalances through a balanced lifestyle or specific nutritional support can help the brain reach the regenerative states it requires to function at its peak.
Cultivating a Sustainable Rest Routine

Prioritizing sleep is a fundamental act of health maintenance. To improve rest quality, experts from the National Sleep Foundation recommend establishing a consistent schedule by going to bed and waking up at the same time daily, even on weekends. Creating a sanctuary for rest is equally important. Maintaining a bedroom temperature between 60 and 67 degrees Fahrenheit and minimizing environmental noise can significantly reduce nighttime disruptions.
Daily physical activity and a dedicated wind-down ritual help signal the brain that it is time to transition from cognitive demands to a state of recovery. By acknowledging that women’s sleep needs are biologically distinct and linked to their high levels of cognitive engagement, households can better support these requirements. Protecting these additional 20 minutes of rest is not an indulgence; it is a necessary investment in long-term physical health and emotional well-being. Prioritizing rest allows the brain to perform the essential repair work required to meet the challenges of each new day with resilience.
Source:
- Scholars@Duke publication: Self-reported symptoms of sleep disturbance and inflammation, coagulation, insulin resistance and psychosocial distress: evidence for gender disparity. (n.d.-b). Scholars@Duke. https://scholars.duke.edu/publication/800861
