Your cart is currently empty!
Researchers Discover Brain Cell Protein That Reverses Memory Decline Without Removing Alzheimer’s Plaques

What if we’ve been chasing the wrong villain in the story of Alzheimer’s?
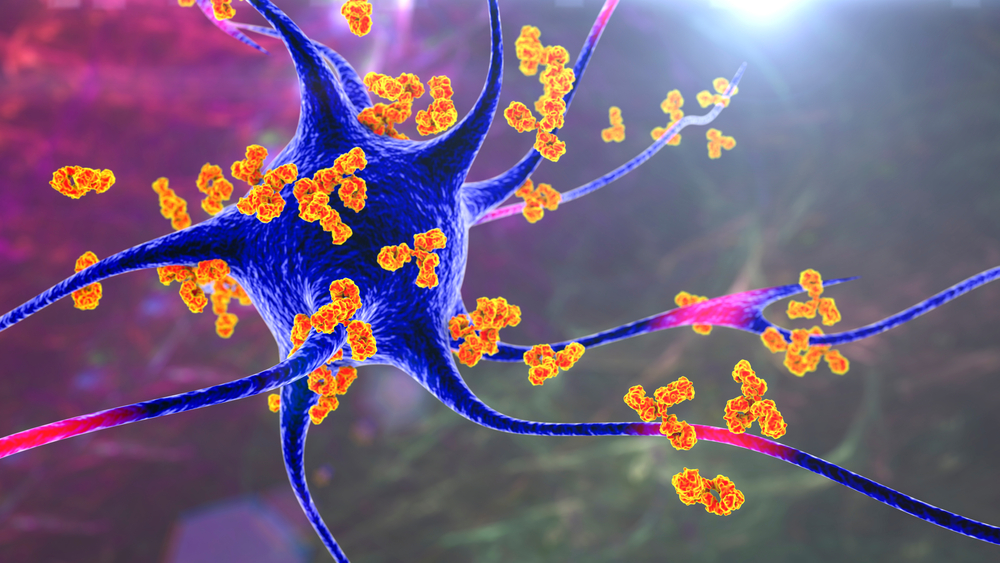
For decades, scientists have zeroed in on the dark buildup of beta-amyloid plaques those sticky protein clumps that gather in the brain as the prime suspect behind memory loss and cognitive decline. Billions have been poured into therapies designed to clear them away, and yet, most have failed to stop the disease’s relentless march. Even when the plaques vanish, memories often don’t return. It’s like cleaning the ashes but never extinguishing the fire.
But a quiet revolution is underway in neuroscience is one that’s not about removing what’s broken, but reigniting what still works. Deep inside the brain, long-overlooked support cells called astrocytes are stepping into the spotlight. And at the center of this shift is a natural protein called hevin, now shown to reverse memory loss in mice without touching a single plaque.
Could healing the brain mean nurturing its inner caretakers instead of attacking its debris?
This is more than just a scientific breakthrough. It’s a reimagining of how we understand aging, resilience, and the biology of memory and it could change the way we fight one of the most feared diseases of our time.
Have We Been Targeting the Wrong Thing?
For years, Alzheimer’s disease has been synonymous with the buildup of beta-amyloid plaques protein fragments that clump between neurons and disrupt communication. These plaques, easily visible under a microscope, have served as both the defining hallmark and the presumed cause of the disease. As a result, most treatment strategies have focused on eliminating them, under the belief that clearing plaques would halt or reverse cognitive decline.
But the results have been sobering.
Despite promising early trials, plaque-targeting drugs have consistently fallen short. While some succeeded in reducing amyloid levels in the brain, very few delivered meaningful improvements in memory or daily function. The puzzling disconnect between reduced plaques and persistent symptoms has raised a critical question in the scientific community: What if amyloid plaques aren’t the main driver of Alzheimer’s after all?
Emerging research suggests that this longstanding assumption may be flawed or at the very least, incomplete. In studies conducted by scientists in Brazil and the United States, animals with Alzheimer’s-like symptoms experienced marked improvements in learning and memory without any reduction in plaque levels. Instead of targeting the visible “debris” of disease, researchers focused on revitalizing the brain’s internal repair systems and saw results.
These findings echo a growing body of evidence indicating that synaptic dysfunction, not plaque presence alone, may be the real engine behind cognitive decline. In other words, the breakdown of communication between neurons how signals are sent, received, and processed could be more important than the mere presence of abnormal proteins.
This shift is not just technical; it’s conceptual. It challenges the notion that brain aging is primarily a process of accumulation and instead points toward dysregulation and cellular exhaustion. Scientists like Dr. Felipe Cabral-Miranda of the Federal University of Rio de Janeiro argue that plaques might be a symptom of a deeper problem, not its cause. “Although cognitive deficits improved significantly, plaque levels remained unchanged,” he noted. “This highlights Alzheimer’s complexity and suggests plaques alone may not be sufficient to cause the disease.”
Astrocytes and Their Vital Role in Brain Health
At the center of this reappraisal is their influence on synapses, the microscopic junctions through which neurons communicate. Synapses are where learning happens, where memories are encoded, and where decline often begins. While neurons fire the signals, astrocytes shape the environment in which that communication occurs. They help form synapses, prune unnecessary connections, and regulate the chemical balance needed for efficient signaling.
When astrocytes falter, so does the entire network.
This is especially relevant in the context of Alzheimer’s disease, where synaptic deterioration not just neuronal death is an early and consistent feature. In fact, the loss of synaptic connections correlates more strongly with cognitive decline than the amount of amyloid plaque present. This suggests that the weakening of communication channels between brain cells could be the true foundation of memory loss.
One molecule in particular has helped shine a spotlight on astrocytes’ importance: hevin (also known as SPARC-like 1). Secreted by astrocytes, hevin plays a key role in assembling and maintaining synapses. It acts almost like a molecular bridge, helping neurons form stable connections essential for memory and learning. In healthy brains, hevin supports the flexible, adaptive networks that allow us to absorb new information and recall the past.
But in the brains of people with Alzheimer’s, hevin levels are consistently lower especially in regions like the hippocampus, which governs memory. This decline in hevin appears to weaken the very scaffolding that supports cognitive function. And it offers a compelling explanation for how dysfunction in these often-overlooked cells could set the stage for the disease.
Flávia Alcantara Gomes, a neuroscientist at the Federal University of Rio de Janeiro, has dedicated years to studying astrocytes’ role in brain aging. “We’ve taken the focus away from neurons,” she says, “shedding light on the role of astrocytes, which we’ve shown could also be a target for new treatment strategies for Alzheimer’s disease and cognitive impairment.”
The Protein That Rebuilds Memory Connections
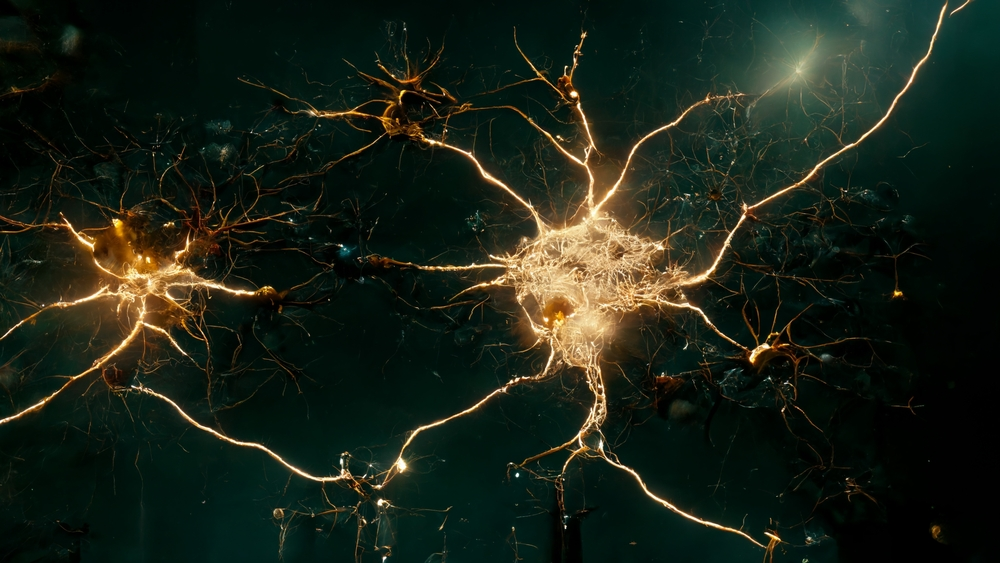
Hevin, also known scientifically as SPARC-like 1, plays a crucial role in synaptogenesis, the process by which new synapses form between neurons. These connections are the foundation of memory, learning, and cognition. When synapses deteriorate as they do in both normal aging and Alzheimer’s disease memory loss often follows. But in recent studies, researchers discovered that increasing hevin levels can actually reverse this process.
In a groundbreaking study by scientists at the Federal University of Rio de Janeiro (UFRJ) and the University of São Paulo, researchers used viral gene therapy to overexpress hevin in the brains of mice genetically engineered to mimic Alzheimer’s disease. These mice were already showing signs of memory decline. Yet, after boosting hevin production specifically in the hippocampal astrocytes, the brain cells that support memory and the animals showed striking improvements in learning and recall tasks.
What made these results even more remarkable was what didn’t change: the amyloid plaques. Despite the return of cognitive function, the characteristic plaques remained in the brain, untouched. This suggested that the cognitive recovery was due not to plaque clearance but to a fundamental rebuilding of synaptic infrastructure an internal rewiring, so to speak.
Advanced proteomic analysis revealed that hevin overexpression influenced dozens of proteins involved in synaptic signaling, structural stability, and neurotransmitter release. In Alzheimer’s-model mice, hevin boosted the expression of key synaptic proteins such as Shank3, Ntrk2, and Cask all essential for maintaining healthy neural communication. In healthy aging mice, similar gains were seen, though through slightly different biological pathways.
These changes weren’t just visible in lab assays they were evident in behavior. Treated mice performed significantly better in a battery of cognitive tasks, including spatial navigation and object recognition. In plain terms: their memories got sharper.
“We found that the overproduction of hevin is capable of reversing cognitive deficits in aged animals by improving the quality of synapses,” said Dr. Flávia Alcantara Gomes, head of the Cellular Neurobiology Laboratory at UFRJ. Her colleague, Dr. Felipe Cabral-Miranda, added that these benefits were observed not only in diseased mice but also in normally aging ones highlighting hevin’s potential to address both pathological and age-related memory loss.
Crucially, the presence of stronger, more mature synapses was confirmed under the microscope. Confocal imaging showed increased overlap between presynaptic and postsynaptic markers visual proof that hevin was enhancing the structural integrity of neural connections.
The Promise of Gene Therapy and Regenerative Medicine
While proteins like hevin are redefining our understanding of how the brain can heal itself, another frontier is pushing this vision even further: gene therapy. Rather than simply introducing helpful molecules, gene therapy works by rewiring the brain’s cells from the inside restoring youthful function to cells already affected by age or disease. And in the fight against Alzheimer’s, this regenerative approach may be as transformative as it is bold.
At the University of California San Diego, neuroscientists have been developing an experimental gene therapy aimed not at clearing amyloid plaques, but at rejuvenating the brain’s own biology. In animal models of Alzheimer’s, this treatment was delivered during the symptomatic stage of the disease to a point when memory loss had already set in. Remarkably, the therapy didn’t just slow further decline; it helped preserve cognitive function and restored key features of healthy brain activity.
This therapy works by altering gene expression patterns in brain cells essentially turning back the cellular clock. Treated neurons began to resemble those found in younger, healthy brains, despite the continued presence of plaques. The implication is profound: if you can reverse the dysfunctional behaviors of cells, you may be able to rescue brain function even in the face of visible pathology.
What makes this approach particularly promising is its potential to act systemically. Unlike plaque-targeting drugs, which aim to remove harmful byproducts, regenerative therapies aim to reset the cellular environment, allowing the brain to repair and reorganize itself. It’s not just defense it’s restoration.
As with the hevin research, these results reinforce a growing scientific shift: that cognitive decline may be more about lost function than irreversible damage. If synaptic communication and cellular health can be restored, then memory and cognition may follow even without removing the plaques that were once thought to be the primary cause.
The UC San Diego therapy has already been licensed to Eikonoklastes Therapeutics and received Orphan Drug Designation from the FDA for its potential in treating ALS, a different but related neurodegenerative disorder. While human trials for Alzheimer’s remain in the distance, this early momentum suggests a wider relevance for age-related brain diseases.
What This Means for the Future of Brain Health
If restoring brain function is possible even without removing the signature markers of disease, then our therapeutic priorities must evolve. Instead of focusing solely on eradicating pathological hallmarks like amyloid plaques, future treatments may aim to enhance the brain’s resilience, restore cellular communication, and rebuild the intricate networks that support cognition.
This opens new avenues for early intervention, particularly in the aging population. While much of Alzheimer’s research has concentrated on late-stage disease, findings from the hevin and gene therapy studies suggest that addressing synaptic and astrocytic health earlier in life even before symptoms emerge—could delay or even prevent cognitive decline. It also reinforces the importance of viewing the brain as a dynamic system, one that can be strengthened and supported, not just shielded from damage.
The broader implications reach beyond Alzheimer’s. The regenerative strategies being explored today could potentially benefit other neurodegenerative disorders like Parkinson’s and ALS as well as general age-related memory loss. And by expanding the focus to glial cells and their molecular tools, scientists may discover more “quiet” players that hold therapeutic promise.
That said, these findings also serve as a reminder of the complexity of the brain. Rebuilding cognition isn’t a matter of flipping a single molecular switch. It requires a systems-level understanding of how neurons, astrocytes, and the proteins they produce interact and how those relationships shift with age, stress, or disease.
For researchers, it means investing in therapies that nurture brain systems rather than just target disease markers. For clinicians and caregivers, it suggests new ways to think about treatment and hope. And for the public, it reframes aging not as a countdown, but as a process with more plasticity and more potential for intervention than we once believed.
The Quiet Revolution in Brain Health
Alzheimer’s has long been seen as an unstoppable force – a slow, irreversible fading of memory and identity. But emerging research is challenging that fatalism. Instead of waging war against plaques alone, scientists are uncovering the brain’s untapped capacity to heal from within, guided by support cells, overlooked proteins, and therapies that restore rather than simply defend.
The discovery of hevin’s regenerative role and the promise of gene therapy mark more than scientific progress; they represent a shift in perspective. They tell us that cognitive decline may not always be the end of the road, but rather a detour—one that future treatments may help reroute. These advances invite us to look at the brain not as a fixed machine prone to failure, but as a dynamic, adaptable ecosystem capable of recovery when given the right tools.
This doesn’t mean cures are just around the corner. Hevin-based therapies and gene-editing technologies remain in the early stages, with challenges like delivery methods, safety, and human testing still ahead. But what has changed irreversibly is our understanding of what’s possible.
As the global burden of dementia continues to rise, these discoveries offer not only scientific promise but emotional relief: that the work being done today could one day restore what once seemed permanently lost. And that perhaps, through science grounded in empathy and innovation, we are finally learning to listen to the brain in all its complexity not just to what breaks, but to what endures and can be rebuilt.
Because sometimes, healing doesn’t begin by fighting harder, it begins by looking in a different direction entirely.
